Nature uses collagen everywhere in constructing multicellular animals. There are at least 20 types of collagen, but 80-90% of the collagen in the body consists of types I, II, and III. Collagen type I is used to form skin, tendon, vascular, ligature, organs, bone, dentin, and interstitial tissues. Collagen type II makes up 50% of all cartilage protein, and is essential in normal formation of such structures as cartilage, the vitreous humor of the eye (the clear gel that fills the space between the lens and the retina of the eyeball of humans and other vertebrates), bones, and teeth. To create these structures, collagen molecules are positioned in arrays called fibrils, producing what are known as the D-periodic fibrillar collagens. Though previous work has given some idea of what the D-periodic structure looks like, technical limitations prevented accurate structural studies of collagen type II packing. A research team aided by the BioCAT 18- ID beamline and the BioCARS 14-BM-C beamline at the APS has remedied that situation by determining the molecular structure of collagen type II in living tissues. These results mark significant progress in understanding the architectural differences between collagen type I and type II. Using these new data, the study of tissue assembly and degradation, such as in osteo- and rheumatoid arthritis, can take several leaps forward.
The special D-periodic arrangement in fibrillar collagens arises when five fragments from five different collagen molecules are arranged to make one complete collagen molecule. Further packing is accomplished, outside of the cell, when multiple fibrils are combined to form fibril bundles. The fibrils themselves are stabilized by cross-linking between collagen molecules facilitated by groups of specific amino acids known as the telopeptides. If the cross-linking is not performed correctly, the resulting instability of the fibrils and tissue can lead to connective tissue diseases, such as glaucoma and arthritis, and to skin fragility in normal aging.
The researchers from the Illinois Institute of Technology performed their investigations on collagen fibrils from the lamprey fish, which electron microscopy shows to be closely related to mammalian fibrils, even though some details of the larger scale architecture differ. The research group had refined their techniques by studying the structure of Type I collagen and then went on to apply those methods to better understand the structure of the more common Type II collagen.
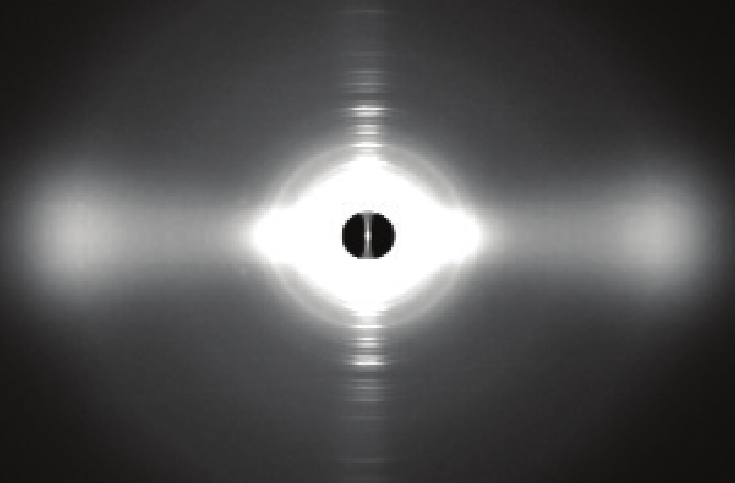
Their major breakthroughs came in conducting x-ray diffraction experiments on whole tissue samples (Fig. 1). Their resulting data on notochord tissue of adult lampreys give a clear picture of the structure of Type II collagen in living tissues. Collagen Type II was chosen for these studies because it shows marked similarity across species, thus allowing starting inferences about its amino acid sequence and broad application of the structures obtained from this study.
By comparing their newly collected data on collagen type II collagen with their previously collected data on collagen type I, the researchers were able to identify critical differences between the molecular packing of the two types of collagen. Their data led them to conclude that these differences in molecular packing may be due to the specific telopeptide shapes in the two molecules. Such information is critical to understanding tissue assembly.
In collagen Type II there is a well ordered cross-linking pattern that is different from that found in collagen Type I. The researchers propose that this finding may explain why collagen Type II differs from Type I in both fibril diameter and fibril bundle organization. The Type II molecule has more amino acids available for cross-linking than does the Type I molecule. This could make the Type II molecule more stable and ubiquitous in network-like tissue formation. But the bulkier nature of the telopeptide component in Type II molecules could also inhibit the formation of Type II molecules as large as those observed for collagen type I.
The diligent work of the research team has provided much needed structural and mechanistic data on collagen fibers. Using these new data, the study of tissue assembly and degradation, such as in osteo- and rheumatoid arthritis, has taken several leaps forward.
See: Olga Antipova and Joseph P. R. O. Orgel, “In Situ D-periodic Molecular Structure of Type II Collagen,” J. Biol. Chem. 285(10), 7087 (March 5, 2010). DOI 10.1074/jbc.M109.060400
BioCAT is a National Institutes of Health supported Research Center (RR-08630). Use of the BioCARS Sector 14 was supported by the National Institutes of Health, National Center for Research Resources, under Grant RR-007707. Use of the Advanced Photon Source at Argonne National Laboratory was supported by the U. S. Department of Energy, Office of Science, Office of Basic Energy Sciences, under Contract No. DE-AC02-06CH1135.
Based on an APS press release by Mona Mort.